At AMHR, it is our mission to deliver state-of-the-art care and meaningful outcomes that impact emotional well-being and addiction recovery. Our mission compels us to take intentional steps to reduce and prevent suicide deaths in our diverse Aurora community. Unfortunately, every year we lose high numbers of community members to suicide.
To meet this challenge, we are integrating the Zero Suicide framework into every aspect of our services. Michell Temple, AMHR’s Suicide Prevention Specialist, and Erin Ralston, Clinical Director, met with me to explain the Zero Suicide framework and the changes it will bring to Aurora Mental Health & Recovery.
Suicide: A Pervasive Problem
Suicide is one of the leading causes of death in the United States. According to the CDC, nearly 46 thousand Americans died by suicide in 2020. And for every death by suicide, they estimate that 275 people seriously considered taking their own life.
Individuals from any demographic group can be impacted, but some groups are at higher risk than others. For example, men are 4 times more likely to die by suicide than women. (Note: This only tells part of the story, as women are more likely to engage in self-harm and suicide attempts.) Nearly half (47.2%) of all deaths by suicide occur among middle-aged adults (35-64 years old). Veterans have an adjusted suicide rate that’s 52.3% higher than non-veterans. Suicide risk is also higher among the LGBTQ+ community.
Zero Suicide: A Revolutionary Answer
According to its website, Zero Suicide is “a way to improve suicide care within health and behavioral health systems”. The reason it’s called Zero Suicide is that “the only acceptable number of losses due to errors in quality of care is zero”. This framework is meant to help organizations apply that mindset to suicide with a system-wide approach.

AMHR Suicide Prevention Specialist, Michell Temple described the Zero Suicide framework as “the current iteration of suicide prevention best practices”. How do we know that’s true? Well, ZS was developed out of a partnership between the National Action Alliance for Suicide Prevention, the Suicide Prevention Resource Center, and other national suicide prevention experts. This specific iteration of best practices has been in development since 2010.
Temple says that with ZS, “what the Suicide Prevention Resource Center has done is laid out a work plan . . . on how an agency can evaluate their current practices to develop a plan to increase their capacity and improve their ability to prevent suicide.” She also made a point to highlight how practical and user-friendly the framework is for evaluating and implementing these best practices. Considering that we’re talking about a system-wide rollout, it’s easy to see how that would be important.
Zero Suicide Effectiveness
An Evidence-Based Approach
The origins of this approach go back to 2001 when Henry Ford Behavioral Health first pioneered the idea of a care pathway to assess and modify suicide risk for patients with depression – setting “zero suicides” as their ultimate goal. Their progress was remarkable as they were able to register zero suicides among patients for 18 months straight in 2009 and 2010.
Since this iteration of ZS rolled out in 2012, the framework has been implemented in over a thousand systems and the evidence of its effectiveness is highly promising.
What makes it so effective?
In Temple’s words, “It’s a community effort . . . And because it has that level of effort and concern for persons who are at risk of suicide, there’s a sense of belonging and connection that actually decreases suicide.”
It seems obvious or even simplistic that when a community of people shows they care, people in that community feel more welcomed and are more likely to reach out for help.
“However, I just want to add that in healthcare it may not be as obvious as we think because not everyone – from the janitor to executives – feels prepared or takes responsibility to respond to a client who may be at risk for suicide. The Zero Suicide initiative really demonstrates a commitment of an agency of 'Everyone needs to be ready'", says Temple. “You need to be ready to demonstrate a community of care for anyone at risk of suicide by transitioning a person to care in a way that makes that person feel they belong – that their life matters.”
How Aurora Mental Health & Recovery Is Implementing Zero Suicide

AMHR’s Clinical Director, Erin Ralston notes that, “we have, as an agency, chosen to take Zero Suicide as our foundational framework for suicide prevention work – recognizing as well that we need to go a couple steps further. And a significant component of that will be integrating Zero Suicide into our very diverse community.”
A Community-First Approach
According to Ralston, “Zero Suicide strongly supports evidence-based practice . . . and we also know that evidence-based practice tends to be biased towards white populations and certain age groups. It leaves out a lot of our BIPOC populations who are greatly impacted by suicide risk. So, for us, Zero Suicide is our foundation and we have these other components that we are also going to address because we need to. This is our community, and we know that those [components] are really important for us.”
As mentioned above, suicide can impact anyone, but some populations are at higher risk than others. In our work as a Certified Community Behavioral Health Clinic (CCBHC) grantee, we are already focused on working with many of the most at-risk groups including those affected by poverty, homelessness, and our refugee populations.
Building a Framework
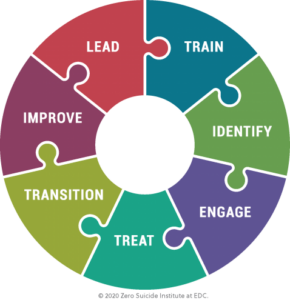
The Zero Suicide framework consists of seven elements: Lead, Train, Identify, Engage, Treat, Transition, and Improve.
- Lead system-wide culture change committed to reducing suicides.
- Train a competent, confident, and caring workforce.
- Identify individuals with suicide risk via comprehensive screening and assessment.
- Engage all individuals at risk of suicide using a suicide care management plan.
- Treat suicidal thoughts and behaviors directly using evidence-based treatments.
- Transition individuals through care with warm hand-offs and supportive contacts.
- Improve policies and procedures through continuous quality improvement.
Early in the process, we created the Suicide Prevention Specialist position (currently occupied by Michell Temple). Her focus up to this point (spring 2023) has been to lay the groundwork for training and implementation.
As she puts it, “We have created what is called a ‘pathway to suicide care’ and it has an initial progression of identification, referral, and assessment. The identification component could impact all employees’ daily interactions with clients of Aurora Mental Health & Recovery because it requires all employees to be prepared to transition a client at risk of suicide to the appropriate clinical staff.”
Training Everyone for Suicide Prevention
AMHR provides a wide range of services with employees in a variety of roles. Each employee will need to receive training that matches the type of role they inhabit and help to move patients to the next step in the process. Ralston explains that there are a couple of ways different agencies go about this:
“One is that you create a singular team that really functions as the suicide prevention specialists. They do that level of care and then you kind of go back to the other teams after they're stable. We've opted for the other version, which is that within all of our teams, we're going to have suicide prevention specialists where when someone is identified, being at that level of risk, we will have evidence-based practices and high-level suicide training on staff within that team to support that client.”
According to Ralston, “The reason we’re setting up for team structure is really that that is the most beneficial to the client. It’s already embedded in the work they’re doing with that team. It maintains that consistency, maintains that engagement, and really helps us deliver the highest possible level of care to that client – where they need it and when they need it – versus any sort of move for them to another team.”
Implementing the Zero Suicide Framework
The truth is that there is no finish line. ZS is an ongoing process. Ralston states, “It is literally embedding a process of continued growth and training and focus on suicide prevention as a foundational value of the agency.” That doesn’t mean there aren’t benchmarks though.
Temple says that “ideally, we are working to have the basic elements of the Zero Suicide framework in place by the end of September [2023].” That’s when the real work starts. From there, AMHR will be focused on constantly improving our policies and practices to better address suicide risk in our community.
How We’re Measuring Success
At this stage, there are two metrics AMHR will be focused on measuring when it comes to our success with the ZS framework. The first should be obvious. It’s mortality. Our goal is to reduce the number of deaths by suicide of clients associated with Aurora Mental Health & Recovery to zero.
The second metric is suicide care management. This will involve measuring clients’ level of satisfaction with their care along with how well we are following our policies and procedures related to that care. Then, based on those factors, we will also be looking at whether and how well we have improved client outcomes.
So, the first metric is focused on suicide mortality across the agency and the second is a measure of client satisfaction and efficacy.
Funding and Support
Ralston is quick to point out that, “suicide prevention, as a whole, is not something that is billable . . . it doesn’t bring in its own revenue.” As important as this work is, suicide prevention is a secondary benefit. It’s foundational to our work, but funding is a challenge.
AMHR received a grant of $104,000 in American Rescue Plan Act (ARPA) funds from Arapahoe County to provide infrastructure needed to “fully adopt the seven principles of the Zero Suicide Framework to better identify suicide risk, train staff on client engagement, implement evidence-based treatments for suicide ideation, and conduct ongoing data collection and measurement.”
That funding is a great start and has allowed us to create the Suicide Prevention Specialist position and begin working through the assessment and planning phases. But Ralston notes that these system-wide changes require a lot of time, effort, and dollars for policy creation, IT implementations, and most importantly – training.
To continue our mission of bringing suicide mortality down to zero, AMHR will be looking for additional grant funding as well as donations from community partners. If you’d like to help, you can donate today here on our website!
A Team Effort
Making system-wide changes in an organization with hundreds of employees is a massive undertaking. Ultimately, implementing this framework will require the help of every single employee at AMHR. However, the team responsible for putting everything in place is composed of just 11 people.
The ZS Implementation Team is made up of AMHR employees who, on top of their other duties, have been meeting every month to facilitate the transition to Zero Suicide. Their commitment to this cause is unrivaled. We thought it was important to acknowledge them here.
Aurora Mental Health & Recovery Zero Suicide Implementation Team (listed in no particular order):
- Erin Ralston, Clinical Director
- Michell Temple, Suicide Prevention Specialist
- Shelley Millsap, Community Connections Vocational Services
- Tiffany Erspamer, Director of Student Training and Clinical Supervision
- Lenard Jones, Youth Specialist (non-clinical) – Aurora Youth Options
- Colton Clark, HRIS Specialist
- Alexis Cislo, Ascent Step-Down Primary Clinician (First Episode Psychosis)
- Jolene Strong, SmartCare- IT (Lead of Zero Suicide from the IT side)
- Lora Wright, Crisis Services
- Vanessa Hudson, Jail-Based Behavioral Health Services
- Thais Kenser Clinical Manager, Child and Family Team - North
On top of all the great work provided by the implementation team, we also have a need for the support and engagement of the Aurora community.
If you would like to learn more about how you can get involved as an AMHR employee, community organization, or even as a community member – please reach out to Erin Ralston, ErinRalston@AuroraMHR.org. We would love to hear from you!